Strategies for Promoting Patient Safety
Medical
errors may occur in different health care settings, and those that happen in
hospitals can have serious consequences. The Agency for Healthcare Research and
Quality, which has sponsored hundreds of patient safety research and
implementation projects, offers these evidence-based tips to prevent adverse
events from occurring in your hospital.
Improve hand hygiene compliance
The link
between dirty hands and the transmission of health care-associated infections has
strong backing in epidemiological literature, and the importance of hand
hygiene has been touted by the World Health Organization, the Joint Commission
and the Centers for Disease Control and Prevention. Yet rates of hand washing
are low, averaging 39%, with many doctors and nurses underestimating the
activity's safety value.Research shows that effective hand hygiene initiatives
improve knowledge of when to clean and how to clean, require demonstration of
the knowledge, ensure that alcohol-based rub and gloves are available at the
bedside, and guarantee that compliance is monitored continuously.
Use barrier precautions to stop the spread of infections
Along with
hand hygiene, barrier precautions are key to reducing the 1.7 million health
care-associated infections that occur in the U.S. each year, which the CDC says
kill about 99,000 patients annually.When a patient has a serious nosocomial
infection such as vancomycin-resistant Enterococcus, health workers should
wear gowns and gloves when providing care. They should use dedicated disposable
equipment and follow the encounter with immediate hand hygiene. A care bundle
including barrier precautions has been shown to cut the spread of VRE from 21%
to 9% in intensive care units.
Avoid hazardous drug abbreviations
About
15,000 medication errors a year have been linked to using abbreviations such as
“u” for “unit” and “q.d.” instead of “once daily.” Starting in April 2004, the
Joint Commission required hospitals to ban these and other commonly used
abbreviations that jeopardize medication safety.Studies done around the time
the ban went into effect found that hospitals were able to cut use of hazardous
medication abbreviations from about 20% to 3% through education and follow-up
with doctors who used the shorthand prescription lingo. Implementation of
computerized physician order entry systems also can help eliminate the vestiges
of this problem.
Use multi component interventions to prevent pressure ulcers
About 2.5
million Americans develop bedsores each year, and about 60,000 patients will
die from complications related to pressure ulcers acquired in U.S.
hospitals.One bundle of preventive care measures has reduced pressure ulcers by
90% at a large health system, from a rate of 5.7% of patients to less than 0.5%.
The bundle, dubbed SKIN, calls for continual assessment of the skin of at-risk
patients, regular turning of these patients, management of incontinence to
prevent soiling that can contribute to bedsores, and nutritional assessment for
malnourishment that can enable the ulcers.
Educate patients about using blood thinners safely
Patients
who have had surgery often leave the hospital with a new prescription for a
blood thinner, such as warfarin brand name: Coumadin®), to keep them from
developing dangerous blood clots. However, if used incorrectly, blood thinners
can cause uncontrollable bleeding and are among the top causes of adverse drug
events. A free 10-minute patient education video and companion 24-page booklet,
both in English and Spanish, help patients understand what to expect when
taking these medicines.
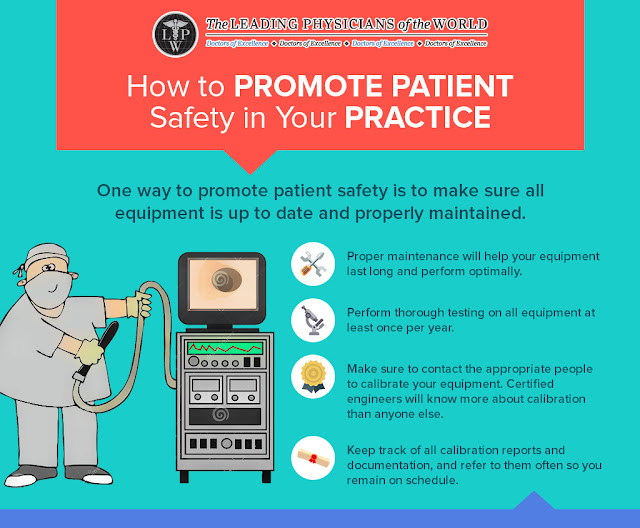
Patient
safety is an essential and vital component of quality nursing care. However,
the nation’s health care system is prone to errors, and can be detrimental to
safe patient care, as a result of basic systems flaws. A variety of
stakeholders are responsible for ensuring that patient care is safely delivered
and that no harm occurs to patients.


Comments
Post a Comment